Shared Insights: The impact of the Covid-19 pandemic on consent
These insights were shared at our fortnightly online forum for NHS professionals on 1 December 2020. To find out more please visit our Shared Insights hub.
Damian Whitlam, a Partner and Amelia Newbold, Risk Management Lead, at Browne Jacobson discussed the legal test codified in Montgomery v Lanarkshire Health Board [2015] and the impact of the COVID-19 pandemic on consent discussions.
Ed Pollard, a Partner at Browne Jacobson specialising in advisory law discussed consent in the context of patients who lack capacity to make a particular decision.
Tim Shurlock, Safety and Learning Lead and Alison Macefield, Associate Safety and Learning Lead shared the data on consent claims.
NHS Resolution has useful consent resources available on its website here.
The Shared Insights were:
Claims data
- NHS Resolution data indicates that there were 2800 claims coded as ‘failure of informed consent’ notified between 2014 and 2019. Of these, 1200 have settled at a total cost (damages and costs) of £208m.
- The most recent data indicates that NHS Resolution is notified of approximately 450 consent claims each year.
- Gynaecology and Orthopaedic claims make up 45% of all consent claims received.
- The NHS Resolution scorecard includes data on consent claims for each individual Trust – for more information, please contact your regional Safety and Learning Lead or contact: safety@resolution.nhs.uk.
The law
- Following Montgomery v Lanarkshire Health Board [2015], clinicians are required to take reasonable care to ensure that patients are aware of any material risks involved in the recommended treatment and any reasonable alternative treatments.
- Determining whether a risk is material to an individual patient requires a two-stage approach involving both objective and subjective assessment:
- what risks would a reasonable person in the patient’s position be likely to attach significance to? and
- what risks should a doctor reasonably be aware that this individual patient would be likely to attach significance to?
The potential impact of COVID-19 on consent discussions
- The challenges posed by the increase in remote consultations and the potential impact on communicating effectively with patients – clinicians need to be confident they have sufficient information to determine what risks are likely to be significant for the individual patient and that the patient has understood the information provided.
- Tool 5 ‘Consent to treatment while COVID is present in society’ published by the Royal College of Surgeons in June 2020 provides practical advice about the specific risks associated with COVID-19. The additional risks associated with Covid-19 should be discussed as part of the consent process and clinicians should be ‘transparent’ about potential and unknown risks.
- The Courts have yet to determine what would constitute reasonable alternative treatment in the context of the pandemic where treatment options may have changed because of the impact on resources and the way in which some treatment is delivered. However, clinicians should discuss how and why any treatment options have changed.
- As ever, the quality of the contemporaneous documentation recording the detail of discussions between clinicians and patients will be key.
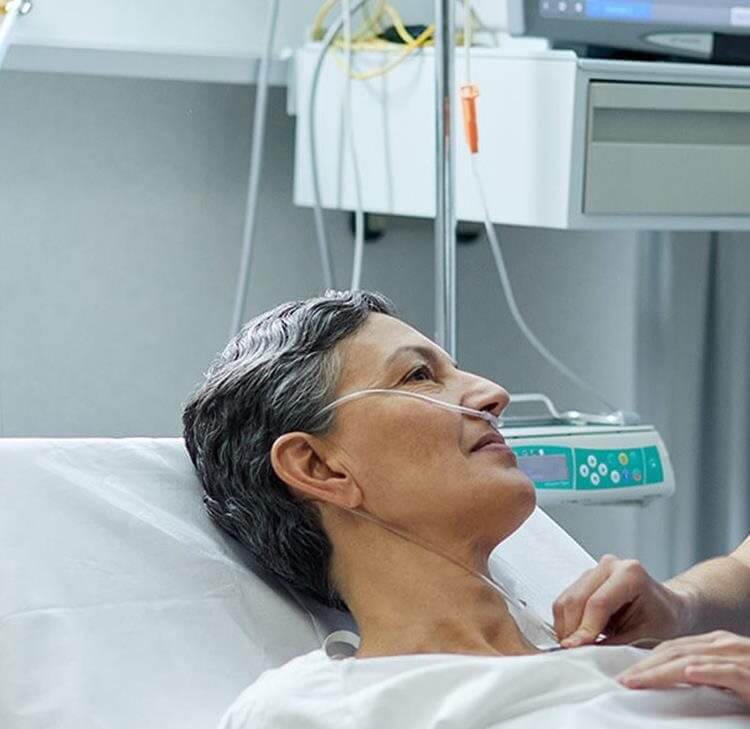
Capacity and consent
- The basic principles are:
- there is an assumption of capacity – you shouldn’t assume someone lacks capacity because of a particular condition they have.
- unwise decisions do not necessarily mean a lack of capacity.
- If a patient is deemed to lack capacity to make a decision about treatment, the best interests process needs to be applied. Best interests is a global assessment, (it is not just about medical issues) and it is person specific
- The Mental Capacity Act sets out the following principles on best interests
- S1(5) – An act done, or decision made, under this Act for on or behalf of a person who lacks capacity must be done, or made, in his best interests
- S1(6) – Before the act is done, or the decision is made, regard must be had to whether the purpose for which it is needed can be as effectively achieved in a way that is less restrictive of the person’s rights and freedom of action.
- Consent is an ongoing process and as the GMC Guidance ‘Decision Making and Consent’ highlights it is important for clinicians to have a number of discussions with the patient, if possible, to allow the patient to consider and reflect upon the information and make a decision. As capacity is decision and time specific, it is important to check on the day of treatment whether anything has changed the patient’s capacity in the intervening period.
- Notes recording capacity decisions should document the decision made and crucially, show how the decision was reached.
Speakers

Amelia Newbold
Risk Management Lead

Ed Pollard
Partner

Damian Whitlam
Partner
Shared Insights
Our monthly forum connecting health and care leaders and professionals to discuss challenges and share solutions.
Contacts

Damian Whitlam
Partner
damian.whitlam@brownejacobson.com
+44 (0)330 045 2332

Nicola Evans
Partner
Nicola.Evans@brownejacobson.com
+44 (0)330 045 2962






![Contractual liability for all inclusive treatment: Bartolomucci v Circle Health Group Limited [2025]](/getattachment/95f9533b-f99c-4fcc-b8d5-3f93904b8242/shutterstock_1265400856.jpg?variant=HeroImageTabletVariantDefinition)